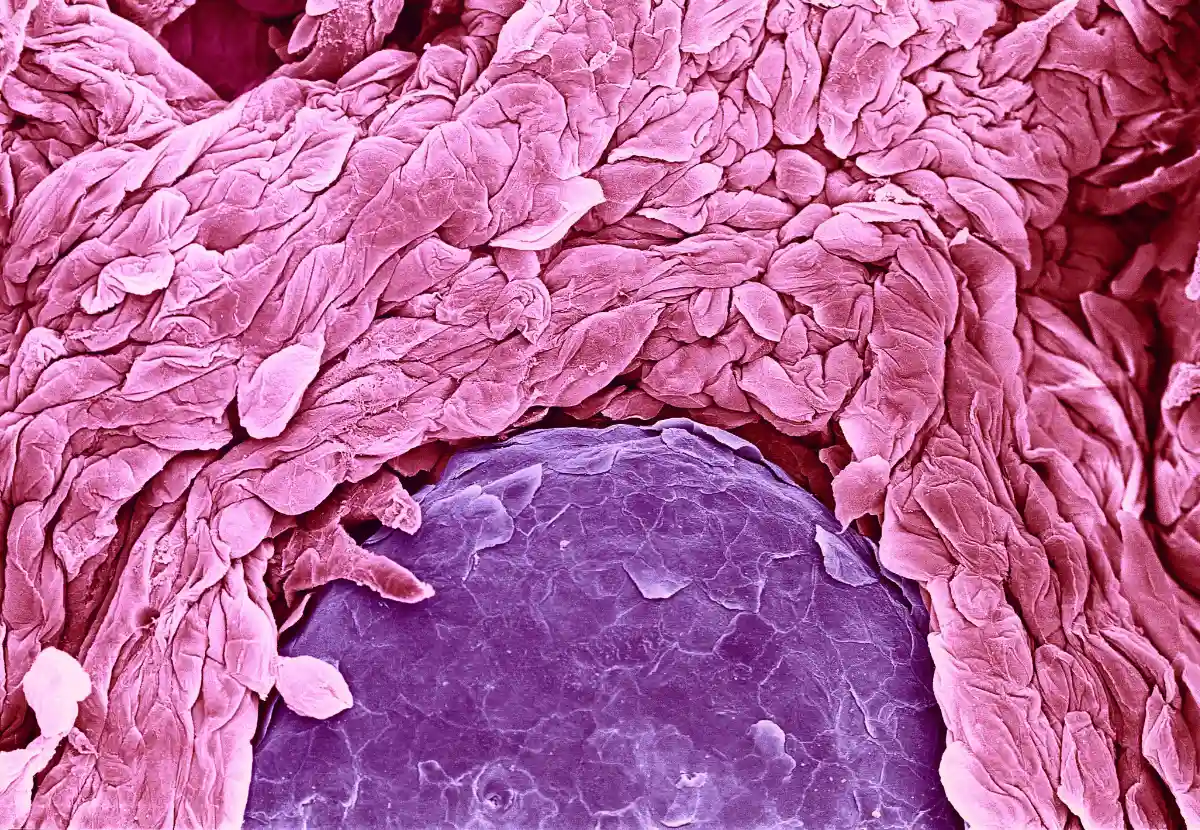
Celiac.com 08/05/2024 – Psoriasis is a prevalent chronic inflammatory skin condition characterized by its autoimmune etiology. Affecting both men and women equally, this disease is often associated with other autoimmune disorders, increasing the complexity of its management. This study aims to explore the prevalence of autoimmune diseases in patients diagnosed with psoriasis at King Abdulaziz Medical City in Riyadh, Saudi Arabia. By identifying these associations, the study provides valuable insights into the interconnected nature of autoimmune conditions.
Study Methods and Patient Selection
The research was conducted as a retrospective, cross-sectional chart review. Patients with confirmed psoriasis diagnoses were identified through the dermatology clinic’s electronic medical records. The charts were meticulously reviewed to document the presence of other autoimmune diseases, including hypothyroidism, hyperthyroidism, alopecia areata, vitiligo, atopic dermatitis, and inflammatory bowel diseases such as Crohn’s disease and celiac disease. Ethical approval was granted by King Abdullah International Medical Research Center’s Institutional Review Board.
Key Findings and Demographic Data
A total of 839 patients were included in the study, with a female majority of 56.4%. The age group with the highest prevalence of psoriasis was between 31 and 50 years, comprising 37.1% of the patients. The study found that 6.8% of the patients had hypothyroidism, making it the most common associated autoimmune disease. This was followed by alopecia areata (3.6%) and atopic dermatitis (2.9%). Rheumatoid arthritis, systemic lupus erythematosus, and inflammatory bowel diseases were notably less common in this cohort.
Discussion on the Association Between Psoriasis and Autoimmune Diseases
The study reveals that a significant number of psoriasis patients also suffer from other autoimmune diseases, with thyroid disorders being the most prevalent. The findings are consistent with other research that suggests a higher susceptibility to autoimmune conditions among psoriasis patients. For instance, autoimmune skin disorders such as alopecia areata and vitiligo were frequently observed. The commonality in immune response mechanisms across these diseases might explain their co-occurrence. In particular, the role of T-cell-mediated processes and cytokine release, such as tumor necrosis factor-alpha and interleukins, is critical in both psoriasis and other autoimmune conditions.
Limitations of the Study
Despite its valuable findings, the study has several limitations. Being a single-center, retrospective study, the results might not be generalizable to other populations. Additionally, the reliance on documented diagnoses in medical records could lead to underreporting or missing data. A larger, multicenter approach would provide a more comprehensive understanding of the prevalence and association of autoimmune diseases with psoriasis.
Implications for Celiac Disease Patients
This study underscores the high prevalence of autoimmune diseases among psoriasis patients, with thyroid disorders and skin autoimmune conditions being the most common. For individuals with celiac disease, these findings are particularly relevant. Understanding the interconnected nature of autoimmune disorders can aid in better managing their health and anticipating potential complications. It also highlights the importance of comprehensive care approaches that address multiple autoimmune conditions simultaneously.
By recognizing these associations, healthcare providers can improve diagnostic accuracy and treatment plans, ultimately enhancing the quality of life for patients with celiac disease and other autoimmune disorders. Further research in diverse populations and larger settings is necessary to validate these findings and expand our understanding of autoimmune disease interactions.
Read more: cureus.com
Source link